The Body Mass Index: A Systematic Review
Stefan Kolimechkov and Lubomir Petrov
How to cite:
Kolimechkov, S. & Petrov, L. (2020). The Body Mass Index: A Systematic Review. Journal of Exercise Physiology and Health, 3(2), 21-27.
Journal of Exercise Physiology and Health
 Iran, Islamic Azad University
Iran, Islamic Azad University
e-mail: jephjournal@gmail.com | website: aiajournals.com/journal/jd/6014
ABOUT THE JOURNAL
The Journal of Exercise Physiology and Health (JEPH) is an international peer-reviewed open access journal published by Azad University (one of the largest comprehensive universities in the world). JEPH publishes high quality research that contributes significantly to the fields of Physiology and Health.
ABOUT THIS ARTICLE
Dr Petrov and I structured this review on the Body Mass Index in a way that provides practitioners and researchers with the tools and information they need, in order to conduct an appropriate weight assessment based on the established international BMI norms.
The Body Mass Index: A Systematic Review
Published Journal Article
Journal of Exercise Physiology and Health
Vol. 3(2), June 2020, pp. 21-27
THE BODY MASS INDEX: A SYSTEMATIC REVIEW
Stefan Kolimechkov and Lubomir Petrov
STK Sport, London, United Kingdom and
National Sports Academy, Sofia, Bulgaria
ABSTRACT
Background: The body mass index (BMI) was described back in 1832 by Adolphe Quetelet and then was validated by Ancel Keys in 1972. BMI is the ratio of body weight expressed in kilograms, divided by height expressed in metres squared. Methods: The aim of this review was to discuss the different criteria used for the assessment of BMI in adults and children, and to provide practitioners and researchers with the tools and information they need based on the established international BMI norms, in order to conduct an appropriate weight assessment. Results: Although the BMI score is calculated in the same way for children and adolescents as the one for adults, the criteria used for weight assessment are different, due to the fact that the BMI in children varies significantly with age. The BMI score in children and adolescents is compared against reference charts for children of the same age and gender, and it is thereby transformed into a percentile score. The assessment of each individual as obese, overweight, normal, underweight, severe thinness is then made based on this percentile score. Discussion: Even though the BMI is the most popular anthropometric index, its main drawback is that it does not distinguish between fat and muscle tissues, and, therefore, the BMI might be an inappropriate method for assessing body weight in some people. Conclusions: It is recommended that BMI is used in combination with other anthropometric parameters for more accurate results when assessing elite athletes, including child athletes.
Keywords: Anthropometry, Body Mass Index, Body Composition
INTRODUCTION
Anthropometry is one of the most widely applied methods to assess the size, proportions and composition of the human body, and it is universally applicable, inexpensive, non-invasive, and can be used to predict health, performance and survival of individuals and populations (1). In order to record accurate results, however, it is essential to follow strict anthropometric data-recording instructions (2, 3).
After the Second World War, the link between human weight and cardiovascular diseases was the subject of many epidemiological studies. The obesity rate increased exponentially over the next few decades, and, therefore, the World Health Organization (WHO) identified this as a global epidemic which threatens public health (4). The WHO reported that overweight / obesity was one of the leading risks for human health (5). Obesity has increased nearly twofold around the world since 1980, with 11% of men and 15% of women being obese in 2014, and about 43 million children under the age of 5 being overweight in 2013, which accounts for more than 1 in 4 children worldwide, according to recent WHO reports (6, 7). In Europe, around one third of children were classified as overweight, and the obesity rate in children and adolescents has increased tenfold since the 1970s (8). The United Kingdom has not only one of the highest obesity rates in Europe, but also amongst all of the other developed countries throughout the world (8-10). Twenty-three percent of children between the ages of 4 and 5, as well as thirty-three percent of those between the ages of 10 and 11, are overweight or obese (9).
What is Body Mass Index (BMI)?
The most appropriate index for determining healthy weight was considered to be the Quetelet index, described back in 1832 by Adolphe Quetelet. He was born on 22 February, 1796 in Ghent (Belgium), and was the fifth of nine children in his family. Adolphe was an exceptionally talented student, receiving many prizes in algebra, geometry, grammar and drawing in secondary school, as well as being the first recipient of a doctorate in science from the University of Ghent at the age of 23 (11). His studies led him to conclude that a person’s weight increases as the square of their height, except during the spurts in growth after birth and during puberty. Subsequently, this concept was known as the Quetelet Index until it was renamedas the Body Mass Index (BMI) in 1972 by Ancel Keys (1904–2004), who confirmed the validity of the index in his research (11, 12).
Today BMI is often used for the classification of a person’s weight as underweight, normal, overweight or obese. Maintaining a healthy body weight throughout a person's lifespan helps maintain good health and reduces the risk of many chronic diseases. The British Government applies BMI as a method for assessing the weight of its population and for promoting a healthy lifestyle (9).
METHODS
The aim of this review was to describe the different criteria used for the assessment of BMI in adults and children, and to provide practitioners and researchers with the tools and information they need, in order to conduct an appropriate weight assessmentbased on the established international BMI norms.
The sources for this systematic review were collected from bibliographic databases (MEDLINE, Google Scholar, Microsoft Academic, PubMed, Web of Science and ResearchGate), reference lists from pertinent review articles and WHO reports up to February 2020. The following keywords were used in various combinations during the electronic searches: body mass index, BMI, assessment, weight, children, adolescents, adults, international norms, limitations, anthropometric index, Quetelet index, athletes. Following a review of titles and abstracts, more than 50 sources were selected, which included original research articles, technical notes, reviews, and WHO reports written in English. The selection of these sources was based on the following inclusion criteria: studies that reported on the development of the international norms of BMI around the world, the methodology used for assessment of BMI in children and adults, as well as the possible limitations or inaccuracy of the BMI.
RESULTS
BMI assessment in adults
The BMI is the ratio of body weight,which is calculated as body weight divided by height in metres squared.
BMI (kg.m-2) = Body weight (kg)* [Body height (m)]-2
For example, for a person with a weight of 66 kg and height of 166 cm, BMI = 66 kg*(1.66 m)-2 = 66*2.76-1 = 23.91kg.m-2
The formula for using pounds and inches is as follows:
BMI (kg.m-2) = 703*Body weight (lb) *[Body height (in)]-2
For example, for a person with a weight of 150 lbs and height of 5’5″ (65″), BMI = 703*[150*(65)-2] = 24.96 kg.m-2
This ratio is then assessed by comparing it to the most commonly used definitions, established by the WHO (13), (Table 1), in order to evaluate a person’s weight: underweight (score of under 18.5 kg.m-2), normal (18.5-24.9 kg.m-2), overweight (25-29.9 kg.m-2) or obese (over 30 kg.m-2).
Table 1: Interpretation of the BMI results [kg.m-2] for adults, established by the WHO (13)
< 18.5 |
Underweight |
18.5–24.9 |
Normal weight |
25.0–29.9 |
Overweight |
30.0–34.9 |
class I Obesity |
35.0–39.9 |
class II Obesity |
≥ 40.0 |
class III Obesity |
BMI assessment in children and adolescents
The BMI score is calculated in the same way for children and adolescents, as for adults. However, the criteria used for weight assessment are different, because the norms for BMI in children vary significantly with age (14-17). For instance, in a new-born child, the BMI median is 13 kg.m-2, and it rises to 17 kg.m-2 for a 1-year-old child, then decreases to 15.5 kg.m-2 for a 6-year-old child, and reaches 21 kg.m-2 for 20-year-old adults (16, 18). Moreover, the amount of body fat changes with age and differs between girls and boys, so BMI age- and gender-specific percentile scores are applied for the accurate assessment of children and adolescents (19).
After calculating the BMI in children and adolescents, the score is then compared against reference charts (Figure1) for children of the same age and gender, and then it is transformed into a percentile or a Z-score (17, 20). For example, if a 10-year-old boy has a percentile score of 95, this means that his BMI is higher than 95 for every 100 boys at the age of 10. Percentile scores, commonly known as 5th, 85th, 95th, 97th percentiles, and Z-scores (-2, +1, +2, etc.) are the most widely applied methods for assessing physical development in children (21). The Z-scores show deviation from the mean value against the reference values and are used interchangeably with the percentile scores (18).
International norms for the assessment of BMI in children and adolescents
In 1993, the WHO reviewed the norms (also called references or curves) for children, published by the National Centre for Health Statistics (NCHS), which were used worldwide as a benchmark from the 1970s. This review showed that changes in the reference curves of the norms were needed in order to present the adequate development in early childhood (22, 23). Moreover, due to some significant technical drawbacks of those norms, it was recommended that they should be updated or replaced (24).
Cole et al. published international norms for the assessment of overweight and obesity in children between the ages of 2 and 18 years (16), but those norms provided only cut-off points without full percentile scores. Then they were adopted by the International Obesity Task Force (IOTF), and subsequently supplemented with cut-off points for estimating underweight levels in children (25). In 2000, the American Center for Disease Control and Prevention (CDC) published American norms with percentile scores for childrenand adolescents (19).
The existence of many different references (NCHS, CDC, IOTF) for the weight assessment in children and adolescents worldwide, as well as their limitations, created a need for the development of new international norms with a full set of percentile scores (26).
From 1997 to 2003, the WHO conducted the Multicentre Growth Reference Study (MGRS), which included children from six different parts of the world: Brazil (South America), Ghana (Africa), India (Asia), Norway (Europe), Oman (Middle East) and the United States of America (North America) (27). The participants in this study were infants and young children < 5 years of age. A strong similarity in the growth and development of the children from different ethnic groups, who were enjoying a similar standard of living, was observed. This justified the inclusion of children from all six selected places and provided uniform international norms for tracking weight and physical development at this age (28, 29). The diet of the participants in the MGRS study was evaluated to be adequate for their needs and physical development (30). Moreover, a high level of reliability of the anthropometric measurements was observed, which was an indicator of the quality of the MGRS study (31, 32).
Prior to the implementation of the new international norms for infants and young children, they were tested in four countries (Argentina, Italy, Maldives and Pakistan), and the data confirmed that the new curves were technically and clinically reliable (33). The WHO published the 2006 MGRS norms for height, weight and BMI, and in 2007 added references for triceps and scapula skin folds and arm circumference (23). When those new WHO norms, based on a sample of healthy infants (34), were compared with the 1977 NCHS norms, it was concluded that the WHO references provided a better tool for monitoring the rapid and changing rate of growth in early infancy (35). The same conclusions were made when comparing the WHO norms with the American (CDC 2000) references (36). In a study on the diagnostic accuracy of the WHO, CDC and IOTF norms, it was found that the WHO reference sseemed to provide a better assessment of overweight and obesity, and the IOTF curves seemed to identify obesity more accurately for Portuguese children (37).
In 2007, the WHO updated the NCHS references for children and adolescents, from 5 and 19 years of age, with new norms, which complied with the existing norms for infants and pre-school children (MGRS), as well as the overweight and obesity curves for 19-year-olds. This provided new international norms with a full set of percentile scores for BMI in children and adolescents (38). The new WHO norms were reported to represent normal physical development under optimal environmental conditions, and, therefore, those references can be applied to assess the weight, growth and development in children from all over the world, regardless of their ethnicity, socioeconomic status or diet (39). By 2011, more than 120 countries around the world adopted these new WHO norms and implemented them in their national programmes (40).
Cole and Lobstein reformulated the IOTF curves for BMI in children from 2 to 18 years of age, and published them as extended international IOTF references, enabling these values to be expressed as percentile and Z-scores (41). A recent study on the similarities and differences between the updated IOTF, CDC and WHO references, concluded that all three classifications showed significant compliance, and, therefore, they could be considered comparable (42).
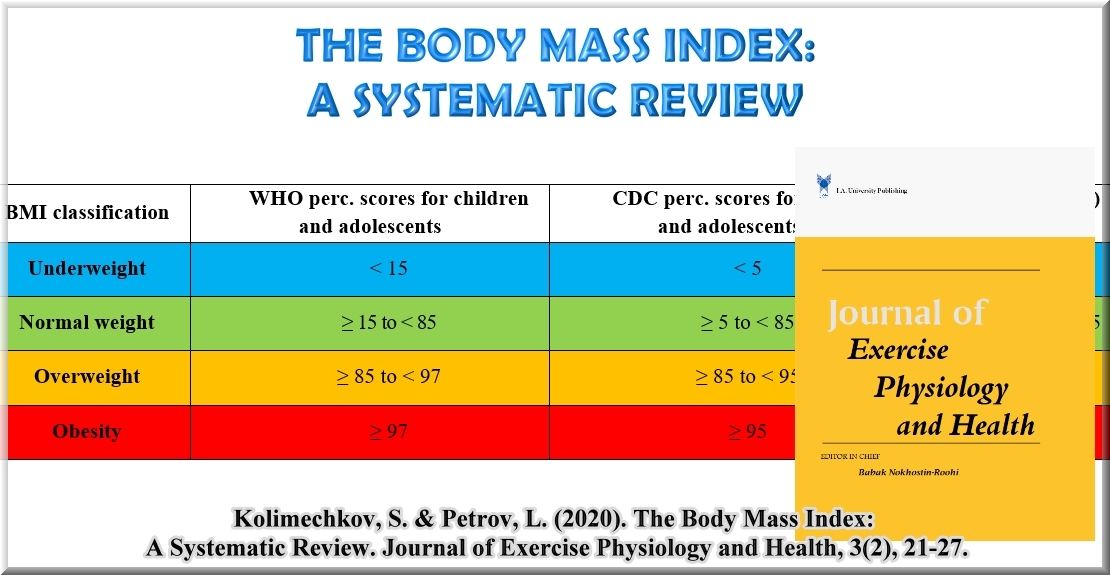
For the assessing of BMI in children and adolescents from 5 to 19 years of age, the WHO provides the following classification: obesity > 97 percentile, overweight 85-97 percentile, underweight <15 percentile, severe thinness < 3 percentile (43). However, the American Center for Disease Control and Prevention (CDC) uses slightly different cut-offs: obesity > 95 percentile, overweight 85-95 percentile, underweight <5 percentile (20). The BMI classification published by the WHO and the CDC is presented in Table 2. In previous American publications, different terminology for children and adolescents (with a percentile score higher than 85 and 95) was employed: overweight risk 85-95 percentile, overweight > 95 percentile (44), but in recent years the term "obesity" (> 95 percentile) has been used (45), and the term "overweight" (85-95 percentile) has been recommended instead of "overweight risk" (46).
Table 2: Classification of the BMI in children, adolescents and adults, according to the American Center for Disease Control and Prevention (CDC) and the World Health Organisation (WHO)
BMI classification |
WHO perc. scores for children and adolescents |
CDC perc. scores for children and adolescents |
BMI (kg.m-2) |
Underweight |
< 15 |
< 5 |
< 18.5 |
Normal weight |
≥ 15 to < 85 |
≥ 5 to < 85 |
≥ 18.5 to < 25 |
Overweight |
≥ 85 to < 97 |
≥ 85 to < 95 |
≥ 25 to < 30 |
Obesity |
≥ 97 |
≥ 95 |
≥ 30 |
The WHO developed comprehensive software programs to enable physical education teachers, sports coaches and sports scientists to track and assess the physical development of children and adolescents. The first release of this software was in 2006 and included "WHO Anthro" for infants and pre-school children, and "WHO AnthroPlus" for children older than 5 years of age. Both software programs are available freely on the official website of the WHO (47). The software automatically calculates the percentile and Z-scores for height, weight, and BMI in accordance with the age and gender of each child, based on the new international norms. The latest version 3.2.2, which is currently in use (47), was released in 2011 (Figure 1).
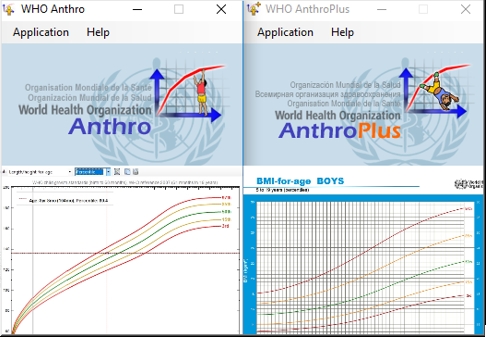
Figure 1: Software "WHO Anthro" and "WHO AnthroPlus" for the calculation of BMI’s percentile and Z-scores of children and adolescents, based on the international norms (47).
DISCUSSION
Although BMI is the most popular and widely preferred anthropometric index (17, 48, 49), its main drawback is that it does not distinguish between fat and muscle tissues. Therefore, some authors reported that BMI might be an inappropriate method for assessing body weight in elite athletes from power sports, people with high levels of physical activity, as well as fitness enthusiasts (12). Garn et al. reported that BMI is highly influenced by body proportions (relative leg length or relative sitting height), in situations where shorter-leg-individuals have higher BMI values by as much as 5 units, and those with narrower chest sizes and longer legs have a lower BMI (50). It has been recommended that BMI be used in combination with other anthropometric parameters for more accurate assessment (51). One such parameter is waist-to-height ratio (WHtR), which has been increasingly used in the assessment of the weight of children and adolescents, because unlike BMI, WHtR is poorly correlated with age, and this reduces the need to use age-specific and gender-specific reference values (52). Body fat percentage as well as parameters for muscle hypertrophy, such as handgrip strength, arm circumference and upper arm muscle area, are also recommended to be considered together with BMI for the assessment of young athletes (53-57).
CONCLUSIONS
BMI is a widely used parameter to assess people’s body weight, and it is often applied in order to promote a healthy lifestyle. The BMI score is assessed by comparing it to the definitions established by the WHO for adults, and by comparing it against age and gender-related reference charts for children. When assessing elite athletes, including children, it is recommended that BMI be used in combination with other anthropometric parameters in order to obtain accurate results.
REFERENCES
1. WHO. Physical status: the use and interpretation of anthropometry. Report of WHO Expert Committiee WHO Technical Report Series 854 Geneva, World Health Organization. 1995http://apps.who.int/iris/bitstream/handle/10665/37003/WHO_TRS_854.pdf?sequence=1.
2. NHNES. National Health and Nutrition Examination survey (NHNES). Anthropometry procedures manual. USA: CDC; 2007. 102 p.
3. Piwoz G, Viteri F. Food and Nutrition Bulletin. UNU. 1985;07(4):86.
4. Eknoyan G. A history of obesity, or how what was good became ugly and then bad. Advances in chronic kidney disease. 2006; 13 (4): 421-7.
5. WHO. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization, 2009
6. WHO. Global Status Report on noncommunicable diseases, World Health Organization. 2014.
7. WHO. Obesity and overweight. Fact sheet no. 311, Jan 2015, World Health Organization: World Health Organization; 2015 [cited 2015 accessed on 27 February]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
8. Branca F, H. Nikogosian, Lobstein T. The challenge of obesity in the WHO European Region and the strategies for response. World Health Organization. 2007.
9. DepartmentofHealth. Healthy Lives, Healthy People: A call to action on obesity in England. 2011.
10. National Obesity Observatory. International comparisons of obesity prevalence. 2009.
11. Eknoyan G. Adolphe Quetelet (1796–1874) - the average man and indices of obesity. Nephrology Dialysis Transplantation. 2007; 23 (1): 47-51
12. Bogin B, Varela-Silva I. The Body Mass Index: the good, the bad and the horrid. Bulletin de la Societe Suisse d'Anthropologie. 2012;18(2):5-11.
13. WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation WHO Technical Report Series 894 Geneva: World Health Organization. 2000.
14. Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Archives of disease in childhood. 1995; 73 (1): 25-9.
15. Holford P, Colson D. Optimum Nutrition for Your Child. Great Britain: Piatkus Books; 2008.
16. Cole T, M. Bellizzi, K. Flegal, Dietz W. Establishing a standard definition for child overweight and obesity worldwide: international survey. Bmj. 2000; 320 (7244): 1240-3.
17. Flegal KM, Tabak CJ, Ogden CL. Overweight in children: definitions and interpretation. Health education research. 2006; 21 (6): 755-60.
18. Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics Series 11, Data from the national health survey. 2002 (246): 1-190.
19. Kuczmarski RJ, Ogden CL, GrummerStrawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: United States. Advance Data. 2000; 314: 1-27.
20. Nihiser A, S. Lee, H. Wechsler, M. McKenna, E. Odom, C. Reinold, et al. Body Mass Index Measurement in Schools, American School Health Association. Journal of School Health. 2007; 77 (No. 10): 651-71.
21. Preedy V. Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease. Wang Y, Chen HJ, editors. London: Springer; 2012.
22. WHO. WHO Child Growth Standards - Methods and development: Head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age. . In: Development DoNfHa, editor. Geneva: World Health Organization; 2007.
23. WHO. WHO Child Growth Standards - Methods and development: Growth velocity based on weight, length and head circumference. In: Development DoNfHa, editor. Geneva: World Health Organization; 2009
24. de Onis M, Yip R. The WHO growth chart: historical considerations and current scientific issues. Bibliotheca nutritio et dieta. 1996 (53): 74-89.
25. Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. Bmj. 2007; 335 (7612): 194.
26. Butte NF, Garza C, de Onis M. Evaluation of the feasibility of international growth standards for school-aged children and adolescents. The Journal of nutrition. 2007; 137 (1): 153-7.
27. WHO. Enrolment and baseline characteristics in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 7-15.
28. WHO. Assessment of differences in linear growth among populations in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 56-65.
29. WHO. Assessment of sex differences and heterogeneity in motor milestone attainment among populations in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 66-75.
30. WHO. Complementary feeding in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 27-37.
31. WHO. Reliability of anthropometric measurements in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 38-46.
32. WHO. Reliability of motor development data in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 47-55.
33. Onyango AW, de Onis M, Caroli M, Shah U, Sguassero Y, Redondo N, et al. Field-testing the WHO child growth standards in four countries. The Journal of nutrition. 2007; 137 (1): 149-52.
34. WHO. Breastfeeding in the WHO Multicentre Growth Reference Study. Acta paediatrica. 2006; 450: 16-26.
35. de Onis M, Onyango AW, Borghi E, Garza C, Yang H, Group WHOMGRS. Comparison of the World Health Organization (WHO) Child Growth Standards and the National Center for Health Statistics/WHO international growth reference: implications for child health programmes. Public health nutrition. 2006; 9 (7): 942-7.
36. de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. The Journal of nutrition. 2007; 137 (1): 144-8.
37. Lopes H. Diagnostic accuracy of CDC, IOTF and WHO criteria for obesity classification, in a Portuguese school-aged children population: Institute of Public Health, University of Porto; 2012.
38. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007; 85 (9): 660-7.
39. WHO. WHO Child Growth Standards based on length/height, weight and age. Acta paediatrica. 2006; 450: 76-85.
40. de Onis M, Onyango A, Borghi E, Siyam A, Blossner M, Lutter C, et al. Worldwide implementation of the WHO Child Growth Standards. Public health nutrition. 2012; 15 (9): 1603-10
41. Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatric obesity. 2012; 7 (4): 284-94.
42. Li K, Haynie D, Palla H, Lipsky L, Iannotti RJ, Simons-Morton B. Assessment of adolescent weight status: Similarities and differences between CDC, IOTF, and WHO references. Preventive medicine. 2016; 87: 151-4.
43. WHO. BMI-for-age (5-19 years): World Health Organization; 2007 [cited 2019 accessed on 19 February]. Available from: http://www.who.int/growthref/who2007_bmi_for_age/en/.
44. Himes JH, Dietz WH. Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive Services. Am J Clin Nutr. 1994; 59 (2): 307-16.
45. Koplan JP, Liverman CT, Kraak VI. Preventing Childhood Obesity: Health in the Balance. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC) 2005.
46. Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007; 120 Suppl 4: S193-228.
47. WHO. WHO Anthro for personal computers, version 3.2.2, 2011: Software for assessing growth and development of the world's children. Geneva: WHO, 2010. 2011.
48. Pekar T. Body Mass Index. IMS Magazine. 2011; Summer 2011: 21-2.
49. Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. Int J Epidemiol. 2014; 43 (3): 655-65.
50. Garn SM, Leonard WR, Hawthorne VM. Three limitations of the body mass index. Am J Clin Nutr. 1986; 44 (6): 996-7.
51. Wilson HJ, Dickinson F, Griffiths PL, Azcorra H, Bogin B, Varela-Silva MI. How useful is BMI in predicting adiposity indicators in a sample of Maya children and women with high levels of stunting? American journal of human biology : the official journal of the Human Biology Council. 2011; 23 (6): 780-9.
52. Taylor RW, Williams SM, Grant AM, Taylor BJ, Goulding A. Predictive ability of waist-to-height in relation to adiposity in children is not improved with age and sex-specific values. Obesity. 2011; 19 (5): 1062-8.
53. Kolimechkov S, Petrov L, Ilinova B, Alexandrova A, Andreeva L, Atanasov P. Assessment of the physical development of pre-school and primary school children practising artistic gymnastics. Journal of Sport Science. 2013; 4: 106-15.
54. Kolimechkov S. Body Mass Index. STK SPORT 2014 [cited Retrieved from https://www.stk-sport.co.uk/sports-science-projects-body-mass-index.html].
55. Kolimechkov S, Petrov L, Alexandrova A, Atanasov P. Nutrition and physical development assessment of pre-school and primary school children practising artistic gymnastics African Journal for Physical Activity and Health Sciences (AJPHES). 2016; 22 (2:2): 565-77.
56. Kiuchukov I, Yanev I, Petrov L, Kolimechkov S, Alexandrova A, Zaykova D, et al. Impact of gymnastics training on the health-related physical fitness of young female and male artistic gymnasts. Science of Gymnastics Journal. 2019; 11 (2): 175 - 87.
57. Kolimechkov S. Physical Fitness Assessment in Children and Adolescents: A Systematic Review. European Journal of Physical Education and Sport Science. 2017; 3 (4): 65-78
Full Text: The Body Mass Index: A Systematic Review. Journal of Exercise Physiology and Health
Available on the official website of the Journal
This article is also available on ResearchGate
Authors
Stefan Kolimechkov PhD
STK Sport, London, United Kingdom
Academia.edu | ORCID | Research Gate | Google Scholar
Associate Professor Dr Lubomir Petrov PhD
Department of Physiology and Biochemistry, National Sports Academy, Sofia, Bulgaria
Academia.edu | ORCID | Research Gate | Google Scholar
Corresponding author: e-mail: dr.stefan.kolimechkov@gmail.com
How to cite this article:
Kolimechkov, S. & Petrov, L. (2020). The Body Mass Index: A Systematic Review. Journal of Exercise Physiology and Health, 3(2), 21-27.